Floods, fires, road accidents, storms, community tragedy - our first responders see a lot. They're on the front line whenever disaster strikes. But how good are we at looking after our emergency workers mental wellbeing? In this episode, you'll hear from two former first responders, both diagnosed with Post Traumatic Stress Disorder (PTSD) and now doing what they can to help others. Find out the role you can play in keeping our emergency workers mentally healthy.
Guest Speakers
 Ross Beckley has 20 years of front line emergency service experience receiving two meritorious service awards and a State Medal for Emergency and Recovery Response. He knows first hand what effects traumatic incidents can have, especially when cumulative. Diagnosed with Post Traumatic Stress Disorder (PTSD) and spending two years in denial, his honest discussions of what can happen when early warning signs of incident stress are ignored led to the launch of Behind The Seen, presentations specifically aimed at the wellbeing of first responders and their families.
Ross Beckley has 20 years of front line emergency service experience receiving two meritorious service awards and a State Medal for Emergency and Recovery Response. He knows first hand what effects traumatic incidents can have, especially when cumulative. Diagnosed with Post Traumatic Stress Disorder (PTSD) and spending two years in denial, his honest discussions of what can happen when early warning signs of incident stress are ignored led to the launch of Behind The Seen, presentations specifically aimed at the wellbeing of first responders and their families.
 John Payne is a veteran who served the Victorian community within Corrections, Government Investigations, and as a Volunteer Firefighter. During a career spanning nearly three decades, John worked on many incidents, including the Black Saturday bushfire of February 2009 for which he was honoured with the National Emergency Medal.
John Payne is a veteran who served the Victorian community within Corrections, Government Investigations, and as a Volunteer Firefighter. During a career spanning nearly three decades, John worked on many incidents, including the Black Saturday bushfire of February 2009 for which he was honoured with the National Emergency Medal.
As a direct result of his service, he was diagnosed with PTSD, a condition he has lived with since 2009.
John wrote ‘What My Eyes Have Seen’, to share his lived experiences with PTSD and is passionate about advocating for mental health and suicide awareness to the greater community and encouraging people to get help.
John hopes his story will help reduce the stigma associated with mental health and increase the understanding of mental health conditions like depression, anxiety and PTSD for first responders, correctional officers, their colleagues, family, and friends. John’s key messages are: ‘Reach out early – you will be supported and don’t suffer in silence.’ Encouraging early help-seeking is a crucial priority in any effective workplace mental health strategy. John is also involved with the following organisations:
• Lived Experience Peer Ambassador
• Beyondblue Speaker
• Founder ‘Talk ‘it’ to Zero’
• Australian & New Zealand Mental Health Association
Steve Carrigg is a registered nurse and has been working in the mental health sector for over 30 years, mostly in rural and remote parts of Australia. Steve is a RAMHP Coordinator based in Lismore. His ‘patch’ is the Northern NSW Local Health District, an area from the Tweed River down to the Clarence River and out west to Tabulam.
is a registered nurse and has been working in the mental health sector for over 30 years, mostly in rural and remote parts of Australia. Steve is a RAMHP Coordinator based in Lismore. His ‘patch’ is the Northern NSW Local Health District, an area from the Tweed River down to the Clarence River and out west to Tabulam.
In his RAMHP role, he has been heavily involved with volunteers, responding to massive floods of 2017 and more recently the Bruxner Highway bushfires in February 2019. He continues to have contact with volunteers from both of these local disasters and greatly respects the role that both spontaneous volunteers like ‘Lismore Helping Hands’ and other longer-established volunteer organisations like the SES and Red Cross play in disaster response and recovery.
Background
First responders are those who are on the front line in disasters, accidents and crisis. While the majority of employee and volunteer first responders have a high level of resilience, they are regularly exposed to traumatic events which can have a profound impact on their mental health.
The workplace environment can also have an influence on the mental health of first responders with inadequate resources and having to work additional unpaid hours along with the impact of gossip, bullying and stigma causing further distress. [1]
There is a range of barriers that may prevent first responders asking for help when needed. These include stigma, wanting to deal with problems themselves, fear of losing the ability to work in an operational role, fear of adverse career impacts or being perceived as weak. Some first responders may not recognise that they are experiencing a mental health problem and so don’t seek support. [1]
Facts and Statistics
Answering the call: Beyond Blue’s National Mental Health and Wellbeing Study of Police and Emergency Services – This report investigates the mental health issues facing our police and emergency personnel.
Beyond Blue. Good practice framework for mental health and wellbeing in first responder organisations – This framework provides first responder organisations with an approach to protect the mental health of their workforce, promote wellbeing and prevent suicide.
NSW Mental Health Commission and the Black Dog Institute. Mental Health and Wellbeing Strategy for First Responder Organisations in NSW – This strategy sets out the commitment of NSW first responder agencies to promote and protect the mental health and wellbeing of their staff and members.
Resources
Black Dog Institute – provides information on post traumatic stress disorder including it’s causes, treatments and how to see help.
SANE – provides a comprehensive factsheet on post traumatic stress disorder.
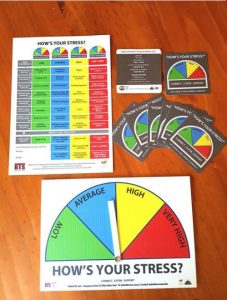
Behind the Seen is working to increase the awareness of incident and career-related stress on first responders and their families. They have a resource pack for first responders, including a tailored version of our ‘How Are You Going?’ poster. www.behindtheseenaustralia.com or www.facebook.com/behindtheseenaustralia/
Help Services
If you or someone else is in immediate danger, call 000 or go to your nearest hospital emergency department.
If you’re concerned about your own or someone else’s mental health, you can call the NSW Mental Health Line 1800 011 511 for advice.
Having a tough time and need someone to talk to right now? The following services are there to listen and help you out. They are confidential and available 24/7.
- Lifeline – 13 11 14
- Suicide Call Back Service– 1300 659 467
- MensLine – 1300 789 978
Online Programs for Post Traumatic Stress Disorder (PTSD):
Mindspot Clinic provides free screening assessments and treatment courses for adults experiencing difficulties with their mental health, including PTSD. The programs also give you the option to contact an online therapist weekly and you get six months further access upon completion.
This Way Up provides online courses for a range of illness experienced by adults including PSTD. These courses cost $60 for 3 months with an additional 12 months access upon completion. This course can be completed with clinician supervision and is available on mobile devices in the app store as well as online.
Mental Health Online provides free information, assessment and treatment programs for adults for a range of mental illnesses including PTSD. The program also gives you the option of using a therapist-assisted program where you will be in contact with an eTherapist.
For Health Professionals
Expert guidelines released by the Black Dog Institute in collaboration with leading clinicians for the diagnosis and treatment of post-traumatic stress disorder in emergency service workers.
Articles
How first responders are coping with PTSD and mental health tolls that come with saving lives
ABC News, 27th June 2019
NSW Fire and Rescue translates research into better mental health for workers
Black Dog Insitute, 12 June 2019